Discover proven RN interview questions plus how CloudApper AI Recruiter automates screening 24/7, cuts time-to-hire by 70%, and finds top nursing talent faster.
Table of Contents
Here’s a sobering reality: the American Hospital Association projects the U.S. will face a shortage of over 200,000 registered nurses by 2031, while healthcare turnover rates have climbed to nearly 26% according to NSI Nursing Solutions. Every day a nursing position remains vacant costs hospitals an average of $1,200 in overtime, agency staffing, and lost productivity. And that’s before we factor in the nightmare of candidate drop-off—SHRM reports that 60% of healthcare candidates abandon applications that take longer than 15 minutes.
The challenge isn’t just finding qualified RNs anymore. Today’s registered nurses need digital fluency with EHR systems, telehealth platforms, and remote patient monitoring tools. They need cultural competency, crisis management skills honed during the pandemic, and the emotional intelligence to handle increasingly complex patient care scenarios. Traditional phone screens and in-person interviews simply can’t keep pace with this demand, especially when you’re competing with every healthcare system in your region for the same talent pool.
That’s where CloudApper AI Recruiter transforms the game. Our conversational AI chatbot engages candidates 24/7 via text or chat, asks these essential screening questions intelligently, and automatically ranks candidates based on their responses—screening 90% faster than traditional methods while eliminating unconscious bias. The system simulates real interviews, adapts follow-up questions based on candidate answers, and integrates seamlessly with your existing ATS.
In this guide, we’ll give you the exact interview questions that separate exceptional RN candidates from average ones, plus show you how AI handles the heavy lifting so your team can focus on what matters: connecting with the best talent and getting them onboarded faster.
Why These Questions Matter for Registered Nurses
The nursing profession has fundamentally transformed over the past five years. Today’s RNs aren’t just providing bedside care—they’re navigating complex technology ecosystems, collaborating across virtual care teams, advocating for patients within value-based care models, and often serving as the critical communication bridge between physicians, specialists, and families. The pandemic accelerated demands for crisis adaptability, mental health awareness, and ethical decision-making under resource constraints.
Old-school questions like “Why do you want to be a nurse?” no longer reveal whether a candidate can thrive in modern healthcare settings. The best RN interview questions now assess clinical judgment in ambiguous situations, comfort with health technology, commitment to continuous learning, and the resilience required for this demanding profession. These questions help you identify nurses who won’t just fill a shift schedule—they’ll elevate your team’s quality of care and stay with your organization for years.
Top 10 Essential Registered Nurse (RN) Interview Questions (With Sample Strong Answers)
1. Describe a situation where you had to prioritize multiple critical patients simultaneously. How did you decide what to do first?
Why ask this? Prioritization and triage skills are the cornerstone of nursing competence, revealing clinical judgment and decision-making under pressure.
Sample Strong Answer:
“During my shift in the cardiac step-down unit, I had three patients who needed immediate attention: one experiencing acute chest pain, another with a rapid drop in oxygen saturation, and a third whose IV had infiltrated with a vesicant medication. I immediately activated the rapid response team for the chest pain patient while delegating the infiltrated IV to our charge nurse who was experienced with vesicant protocols. I personally addressed the oxygen saturation issue because I could quickly assess and intervene—turned out to be a simple issue with the patient’s positioning. Within four minutes, all three situations were being managed appropriately. I used the ABCDE priority framework—Airway, Breathing, Circulation first—but also considered what resources I could leverage and delegate effectively.”
2. Tell me about your experience with Electronic Health Records. Which systems have you used, and how do you ensure documentation accuracy when you’re extremely busy?
Why ask this? EHR proficiency is non-negotiable in modern healthcare, and this reveals both technical competence and documentation discipline.
Sample Strong Answer:
“I’ve worked extensively with Epic and Cerner over the past four years. I’m comfortable with medication reconciliation modules, charting by exception, and using clinical decision support tools embedded in the systems. When things get hectic, I use a hybrid approach—I jot quick notes on my SBAR pocket card during the immediate situation, then I document in real-time during any transition moments, like when waiting for medications from pharmacy or during brief lulls. I also use voice-to-text features for narrative notes when appropriate. I’ve learned that trying to document everything from memory at shift end leads to errors and omissions, so I’ve trained myself to find those 30-second windows throughout the shift. Accurate documentation isn’t just compliance—it’s patient safety and legal protection for everyone.”
3. How do you handle situations where a patient or family member refuses a treatment that you know is medically necessary?
Why ask this? This tests patient advocacy skills, ethical reasoning, and communication abilities—all critical for patient-centered care.
Sample Strong Answer:
“First, I always seek to understand the ‘why’ behind the refusal through open-ended questions and active listening. Often there’s a knowledge gap, a previous bad experience, or cultural or religious considerations I’m not aware of. For example, I once had a diabetic patient refusing insulin because they feared ‘becoming dependent’ on it. I took time to explain the pathophysiology in simple terms, acknowledged their concern as valid, and brought in our diabetic educator for additional support. We also involved the physician to discuss alternative approaches. Ultimately, it’s about informed consent—my job is to ensure they truly understand the risks of refusal, provide all the information they need, document thoroughly, and respect their autonomy while advocating for their health. If there’s ever a capacity concern, I involve our ethics committee.”
4. Describe your approach to preventing medication errors, especially during high-stress situations.
Why ask this? Medication safety is paramount, and this reveals systematic thinking and commitment to evidence-based protocols.
Sample Strong Answer:
“I follow the ‘seven rights’ religiously—right patient, drug, dose, route, time, documentation, and reason—even when I feel rushed, because shortcuts are when errors happen. I use barcode scanning verification for every medication administration, and I’ve developed a personal habit of verbalizing the medication name and patient identifier out loud before administration, even if no one else is in the room. During emergencies or codes, I employ the ‘repeat-back’ method with physicians for any verbal orders and have a colleague verify high-alert medications like insulin or heparin when possible. I also believe in speaking up about near-misses during our unit safety huddles—those learning moments have prevented actual errors. Technology helps tremendously, but human vigilance and a safety culture are irreplaceable.”
5. How do you stay current with evolving clinical guidelines and nursing best practices?
Why ask this? Healthcare evolves rapidly; you need nurses committed to lifelong learning and professional development.
Sample Strong Answer:
“I maintain my professional development through multiple channels. I’m an active member of the American Nurses Association and subscribe to their nursing journals—I particularly follow updates on evidence-based practice guidelines. I complete continuing education through my hospital’s learning management system and outside sources like Medscape and NursingCE. I also attend our unit’s monthly journal clubs where we discuss recent research and how to implement changes in practice. Recently, I completed a certification in critical care nursing through AACN, which required staying updated on the latest sepsis protocols and ventilator management strategies. I also learn from my colleagues—our unit has nurses with specialized knowledge, and I make it a point to ask questions and shadow when new procedures are introduced.”
6. Tell me about a time you identified a patient safety issue that others had missed. What did you do?
Why ask this? This assesses clinical observation skills, critical thinking, and willingness to speak up—all hallmarks of excellent nurses.
Sample Strong Answer:
“I was admitting a post-surgical patient whose vital signs were technically within normal limits, but something felt ‘off’ to me. His heart rate was trending upward, he seemed anxious, and his skin had a subtle grayish tone that wasn’t documented in the transfer notes. Rather than dismiss my gut feeling, I did a thorough head-to-toe assessment and noticed diminished breath sounds on his operative side. I immediately notified the surgeon, who ordered a stat chest X-ray that revealed a developing pneumothorax that needed immediate intervention with a chest tube. That experience reinforced for me that nursing intuition combined with systematic assessment can be lifesaving. I always trust that feeling that something isn’t right and investigate further rather than assuming everything is fine just because it looks okay on paper.”
7. How do you manage the emotional toll of nursing, especially after difficult patient outcomes or long stretches of high-acuity shifts?
Why ask this? Burnout and compassion fatigue are epidemic in nursing; you need candidates with self-awareness and healthy coping strategies.
Sample Strong Answer:
“I’ve learned that self-care isn’t selfish—it’s essential for providing quality patient care long-term. After particularly difficult shifts, I use the drive home to decompress and mentally transition out of work mode. I’m part of a peer support group at my current hospital where we can process difficult cases in a confidential setting, which has been invaluable. Physically, I prioritize sleep, exercise, and nutrition—when I let those slip, I notice my resilience drops significantly. I also practice boundary-setting, like not checking work emails on my days off unless I’m on-call. I’ve learned to celebrate the small wins and focus on the patients we did help, rather than dwelling exclusively on the ones we lost. And honestly, I’m not afraid to use our EAP counseling services when I need professional support—mental health matters for healthcare workers too.”
8. Describe your experience working with diverse patient populations. How do you ensure culturally competent care?
Why ask this? Healthcare disparities are a critical issue; culturally competent nurses provide better outcomes for all patients.
Sample Strong Answer:
“In my previous role at an urban medical center, I cared for patients from over 40 different countries and language backgrounds. I’ve learned that cultural competence starts with humility—recognizing that I don’t know everything about someone’s cultural health beliefs and being willing to ask and learn. I routinely use interpreter services for non-English speaking patients rather than relying on family members, which protects patient privacy and ensures accurate communication. I’ve also educated myself on common cultural considerations around pain expression, family involvement in decision-making, dietary restrictions, and end-of-life preferences for the populations we serve most frequently. But I never make assumptions—I treat every patient as an individual and ask open-ended questions about their preferences, beliefs, and what’s important to them in their care.”
9. How would you handle a situation where you disagreed with a physician’s order that you believed could harm the patient?
Why ask this? This tests advocacy, professional courage, and understanding of nursing scope of practice.
Sample Strong Answer:
“As a nurse, I’m the last line of defense for patient safety, so I take this responsibility seriously. If I believed an order could cause harm, I would first verify I understood it correctly—sometimes it’s a communication issue. If my concern remained, I’d respectfully contact the physician directly, stating my specific concern using SBAR format: ‘I’m calling about patient X, their current situation is Y, my assessment shows Z, and I’m concerned this order might cause W effect because…’ Most physicians appreciate nursing input, and often we can problem-solve together. If the physician insisted and I still believed it was unsafe, I’d follow my hospital’s chain-of-command protocol—involving the charge nurse, nursing supervisor, and potentially the patient safety officer. I’d also document my concerns and the steps I took. Patient safety supersedes hierarchy, and any reputable healthcare organization supports nurses who advocate appropriately.”
10. What experience do you have with telehealth or remote patient monitoring? How comfortable are you with these technologies?
Why ask this? Virtual care is expanding rapidly; nurses must adapt to delivering care through digital platforms.
Sample Strong Answer:
“During the pandemic, our unit transitioned to hybrid care with telehealth rounding for stable post-op patients, which gave me significant exposure to virtual care delivery. I became comfortable conducting video assessments, coaching patients through self-examination techniques, and identifying when in-person evaluation was necessary despite technological limitations. I’ve also worked with remote monitoring devices for heart failure patients—reviewing their daily weight, BP, and symptom data, then doing telephonic follow-up. The key difference I’ve learned is over-communication and very clear, specific instructions, since you can’t physically demonstrate or touch the patient. I’m genuinely excited about these technologies because they improve access to care, but I’m also realistic about their limitations and when traditional bedside nursing is irreplaceable.”
How CloudApper AI Recruiter Makes Hiring Registered Nurses Effortless
Here’s the challenge every healthcare HR team faces: you need to screen dozens of RN candidates quickly, ask consistent, role-specific questions, and identify top talent before competitors snatch them up—all while your recruiting team is already underwater with other open positions.
CloudApper AI Recruiter solves this by deploying a conversational AI chatbot that engages candidates the moment they express interest—via SMS text or web chat—and conducts intelligent screening interviews 24/7, asking exactly these types of questions (or your customized versions) in a natural, conversational flow.
Here’s how it specifically transforms RN hiring:
Automated Clinical Competency Screening
The AI asks technical questions about medication administration, patient prioritization, EHR systems, and specific nursing specialties (ICU, ER, Med-Surg, etc.), then evaluates responses using healthcare-specific keywords and competency frameworks your team configures.
Instant Engagement = Zero Drop-Off
When an RN applies at 11 PM after their shift (prime healthcare candidate time), CloudApper immediately engages them via text. No waiting 3 days for your recruiter to call. Candidates complete screening in 10-15 minutes on their phone, and your team wakes up to ranked, qualified applicants ready for manager interviews.
Bias-Free, Consistent Evaluation
Every candidate gets asked the same core questions in the same way. The AI scores responses objectively based on criteria you define—clinical knowledge, cultural fit indicators, scheduling flexibility, license verification—eliminating the unconscious bias that creeps into traditional phone screens.
Healthcare-Specific Question Libraries
CloudApper comes pre-loaded with validated questions for nursing specialties, but you can customize everything. Want to ask about your specific EHR system? Particular unit protocols? Shift preferences? The AI adapts the conversation flow based on candidate responses, asking intelligent follow-ups just like a skilled recruiter would.
Seamless ATS Integration
All candidate data, conversation transcripts, and screening scores feed directly into your existing applicant tracking system—Workday, Greenhouse, Taleo, you name it. No manual data entry, no switching between platforms.
Real Results for Healthcare Organizations
A 300-bed hospital system in the Midwest implemented CloudApper AI Recruiter for their RN hiring and reduced time-to-hire by 68%—from an average of 42 days down to just 13 days. Their talent acquisition team went from conducting 200+ phone screens monthly to focusing exclusively on in-person interviews with pre-qualified candidates. Candidate satisfaction scores increased because nurses appreciated the respectful, immediate engagement rather than playing phone tag for weeks.
The platform also handles all the administrative heavy lifting: automated interview scheduling with your hiring managers, license verification reminders, reference check coordination, and even onboarding document collection—all through conversational AI that feels human, not robotic.
Stop losing qualified RN candidates to faster competitors. Let CloudApper handle the initial screening so your team can focus on the high-value conversations that actually require human judgment and relationship-building.
Ready to Transform Your RN Hiring Process?
The nursing shortage isn’t going away, but your hiring timeline can shrink dramatically with the right technology. These 10 essential interview questions give you a framework for identifying exceptional registered nurses—and CloudApper AI Recruiter automates the entire process of asking them, screening candidates, and delivering qualified talent to your hiring managers 10× faster.
Book a personalized demo today and see how our AI chatbot can engage your next great RN within minutes of application, not days. Your talent acquisition team will thank you, your hiring managers will thank you, and most importantly, your patients will benefit from getting exceptional nurses on the floor faster.
Schedule your CloudApper AI Recruiter demo now →
What interview questions have worked best for your RN hiring? Drop a comment below—we’d love to hear what’s working for healthcare recruiters.
You might also like to read:
10 Essential Home Health Aide & Phlebotomist Interview Questions (+ AI Recruiter Automation Guide)
10 Essential CNA & Patient Care Tech Interview Questions to Ask (And How AI Makes Hiring 10× Faster)
10 Essential Medical Assistant Interview Questions to Ask (Plus How AI Recruiter Can Automate The Entire Hiring Process)
What is CloudApper AI Platform?
CloudApper AI is an advanced platform that enables organizations to integrate AI into their existing enterprise systems effortlessly, without the need for technical expertise, costly development, or upgrading the underlying infrastructure. By transforming legacy systems into AI-capable solutions, CloudApper allows companies to harness the power of Generative AI quickly and efficiently. This approach has been successfully implemented with leading systems like UKG, Workday, Oracle, Paradox, Amazon AWS Bedrock and can be applied across various industries, helping businesses enhance productivity, automate processes, and gain deeper insights without the usual complexities. With CloudApper AI, you can start experiencing the transformative benefits of AI today. Learn More
CloudApper AI Solutions for HR



- Works with
- and more.
Similar Posts

How cNPS Reflects Your Recruitment and Employer Brand
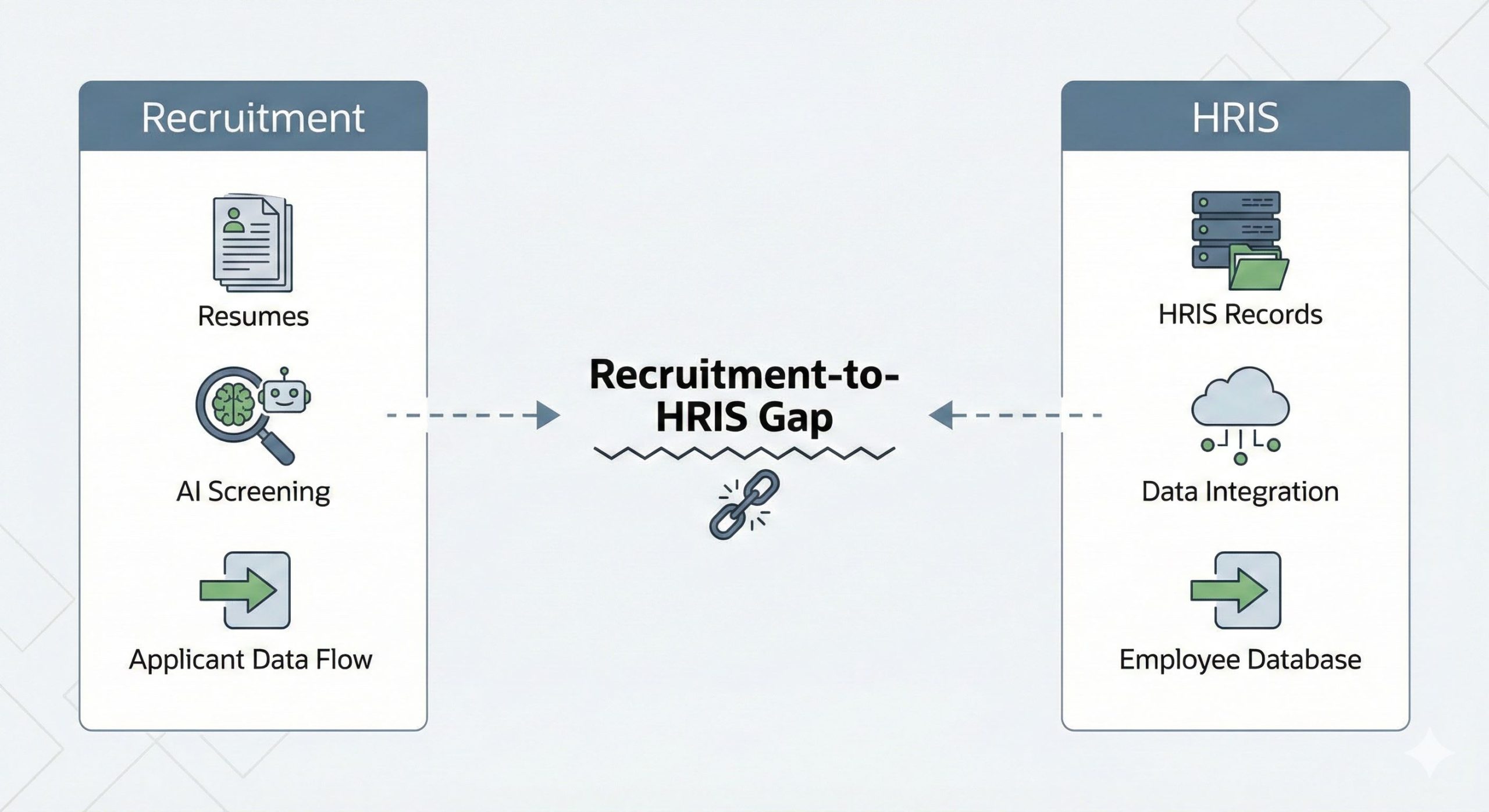
The Recruitment-to-HRIS Gap: Why Your “System of Record” Should Start…